What are the 17 PTSD Signs and Symptoms?

If you're asking yourself, "Do I have PTSD?" start by taking our free quiz.
Spotting the signs and symptoms of PTSD can be difficult. Research suggests that only 2-11% of people experiencing trauma symptoms are actually diagnosed.1 This is one of the many reasons Stella is dedicated to the education of the impact of emotional trauma and the available treatment options. We strongly believe that demystifying the impact and treatment of trauma reduces stigmas associated with PTSD.
While PTSD has been referred to as a disorder, many claim it's an injury. Stella and others have suggested a new term – Post Traumatic Stress Injury (PSTI) – in place of Post Traumatic Stress Disorder (PTSD)2.
What Are the 17 Symptoms of PTSD?
Trauma can cause symptoms that diminish our capacity to experience warm and loving feelings from others (i.e., emotional numbness), which can lead to profound negative changes to our self-image and identity and spark fears that often limit our enjoyment of pleasurable activities. When we have symptoms following trauma exposure, we may have recurring feelings of helplessness and horror. We also commonly experience panic attacks, feelings of self-blame and shame, chronically disrupted sleep, and relationship conflicts with loved ones.
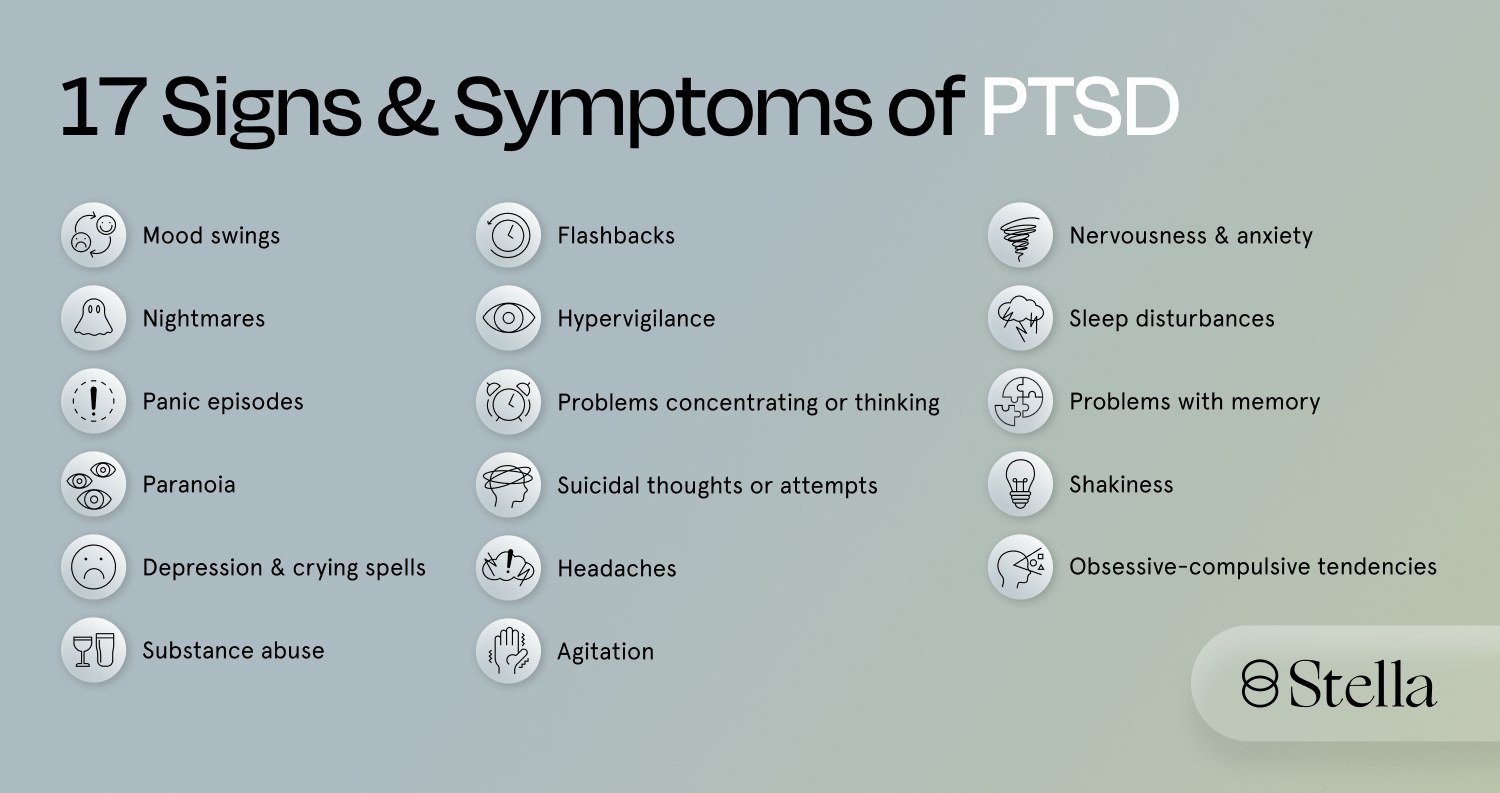
The 17 symptoms of PTSD are:
- Agitation
- Nervousness & Anxiety
- Problems with Concentration or Thinking
- Problems with Memory
- Headaches
- Depression & Crying Spells
- Suicidal Thoughts or Attempts
- Mood Swings
- Obsessive-Compulsive Tendencies
- Panic Episodes
- Paranoia
- Shakiness
- Substance Abuse
- Flashbacks
- Hypervigilance
- Nightmares
- Sleep Disturbances
Read on to learn more about the 17 most common symptoms.
1. Agitation
Agitation is a feeling of anxiety or nervous excitement. Like many symptoms experienced after trauma, agitation is understood on a spectrum. Words like restless, uneasy, and tense generally describe mild agitation. When we're agitated, we may be fidgety or find it hard to sit still. Agitation can build to the point that we've become short-tempered or continually irritable. Untreated trauma can contribute to aggressive or harmful behavior toward ourselves or others.
2. Nervousness and anxiety
It's normal to worry about stressful situations (like a job interview or putting an offer in on a house) before they happen. But when we experience symptoms following trauma exposure, these nervous feelings are persistent and all-consuming to the point that they disrupt everyday life. Tense, worried thoughts often manifest physically. For example, when we're exposed to trauma and experience anxiety, we might have an increased heart rate, breathe rapidly, sweat, or feel tired.
3. Problems with concentration or thinking
The body's fight-or-flight response turns on when we experience trauma or a very stressful event. And sometimes it stays on long after the traumatic event, which can make us feel like we need to be on constant high alert. This, in turn, makes it challenging to concentrate or think clearly.
4. Problems with memory
After experiencing trauma, the fight-or-flight response may become "stuck" in an over-activated state that causes nerve growth around the amygdala (also known as the brain's "fear center").3 The amygdala – along with the hippocampus and prefrontal cortex – plays a role in the brain's ability to process stress and memory. Memory loss can also occur as a defense mechanism.
5. Headaches
When the fight-or-flight trauma response is triggered, the body releases cortisol and adrenaline – two hormones that help it respond to a threat. When we experience symptoms of trauma, our fight-or-flight response can become locked into a continually activated state, and, in this state, our bodies produce hormones that can impact the body's nervous system, sometimes resulting in headaches4. Headaches can have many other causes, but can still be a symptom of PTSD especially when combined with other symptoms.
6.Depression and crying spells
Depression negatively impacts how we think and feel about ourselves. It can also influence the way we behave. When we are exposed to trauma and experience depression, we may feel sad, lose interest in activities we enjoyed before their trauma, feel guilty and worthless or notice changes in our appetite. Depression can also cause increased fatigue and disrupted sleep – we might have trouble sleeping while others sleep too much. At its worst, depression can lead to suicidal ideation.
7. Suicidal thoughts or attempts
We can be so overwhelmed by our PTSD symptoms that we sometimes consider harming ourselves or suicide. When we're experiencing trauma symptoms, we can also experience depression, panic attacks, anxiety, and substance abuse and are at higher risk for suicide. In fact, people diagnosed with trauma symptoms are 9.8 times more likely to die by suicide.5
If you are thinking about suicide or need emotional support, please text "HOME" to 741741 for free, 24/7 crisis counseling from Crisis Text Line. We want you to know that you are not alone and that there is hope.
8. Mood swings
Trauma triggers and other common experiences like panic attacks and bursts of irritability can cause sudden mood changes following trauma exposure. While bipolar disorder is a different condition, the mood swings that come with trauma exposure may sometimes be mistaken for bipolar disorder, and in some cases, we may have both conditions. Working with a licensed clinician is the key to figuring out the right diagnosis.
9. Obsessive-compulsive tendencies
While being diagnosed with trauma symptoms and Obsessive-Compulsive Disorder (OCD) are different conditions, after we're exposed to trauma, we may behave in ways that look similar to OCD. For example, we may check the locks on their doors several times before leaving the house in response to the hypervigilance that can come after a trauma.
OCD and those diagnosed with trauma symptoms can both suffer from intrusive, disturbing thoughts. When we experience both conditions, we often feel a constant impending sense of doom or dread. This can be a sign of PTSD especially if you previously did not have any sort of OCD.
10. Panic episodes
Feeling afraid is common when we're exposed to trauma. When we are suddenly overwhelmed with intense fear, it could mean that we are experiencing a panic attack. Sometimes these episodes seem to come without warning or reason. Other times, they happen in response to a reminder of our trauma.
During a panic attack, we may feel like we're not in control of ourselves or afraid of dying. Chest pain, trembling, hot flashes or chills, a choking sensation, and other physical symptoms are commonly associated with panic attacks.
11. Paranoia
Paranoia is another one of the 17 symptoms of PTSD. In reaction to traumatic or highly stressful events, we can become paranoid. Our belief that we are unsafe causes us to act highly guarded and suspicious of others. We adopt this way of thinking to protect ourselves from being harmed or harassed.
12. Shakiness
Shakiness is related to many common trauma symptoms like agitation, nervousness, anxiety, panic episodes, and substance abuse.
13. Substance abuse
When experiencing symptoms following trauma, we may use drugs and alcohol to cope as taking substances can temporarily reduce or numb the upsetting feelings we're experiencing.
14. Flashbacks
Flashbacks are vivid re-experiencing of partial or full aspects of past traumatic events or stressors as if they are happening in the present moment. When flashbacks happen, it can feel uncontrollable and terrifying. Most flashbacks can come on in the forms of images, like watching a video of what happened. But in some cases, many relive other sensations of the trauma like the sounds, smells, tastes, or feeling a physical pain or pressure. Moreover, some you may re-experience the emotions that you felt during the traumatic events. Sometimes flashbacks are triggered, but they can also happen randomly. The duration of a flashback can vary from seconds to several hours, and it can often be accompanied by other physical symptoms like sweating and an increased heart rate.
15. Hypervigilance
Hypervigilance is common for those who experienced trauma and stressors. It is characterized by a heightened and sustained state of alertness of potential threats as an adaptive response that initially serves as a way of protecting oneself. People experiencing hypervigilance may be constantly scanning their surroundings, expecting something bad to happen. They may be on edge or jumpy, overreacting to things or stimuli happening around them.
16. Nightmares
Trauma can manifest in the form of vivid dreams that often replay the traumatic events from the past. Those who are experiencing nightmares may feel a sense of intense fear, horror and helplessness as if they are still reliving the traumatic events. It can lead to sleep disturbance or cause people to be afraid of going to sleep. It can also cause an overwhelming emotion of anxiety, anger, or sadness upon their waking, or lead to fatigue in the daytime.
17. Sleep Disturbances
Individuals may have difficulties falling asleep or staying asleep due to intrusive and distressing memories from the past resurface during the night. Sleep may also be disturbed by frequent nightmares and night terrors. As a result, some individuals may develop sleep avoidance, which leads to long-term sleep deprivation that may further exacerbate other symptoms of PTSD. Disrupted sleep significantly impairs mood and performance during the daytime, like difficulties concentrating, decreased productivity, lower quality of life, negative impact on close relationships and increased health risks.
Treating PTSD Symptoms with Stella
In recent years, the Stellate Ganglion Block (SGB) has emerged as a promising treatment option for symptoms of trauma. Stella founders Dr. Eugene Lipov and Dr. Shauna Springer recently published a study with other trauma experts that indicates that the Stellate Ganglion Block (SGB) is an effective treatment for PTSD symptoms regardless of gender, trauma type, PTSD-related medication use, history of suicide attempt, or age.6
Stellate Ganglion Block (SGB) by Stella has the potential to help millions of people with emotional trauma experience lasting relief. To learn more, please visit our "How It Works" page.
If you want to learn more about Treatment by Stella call our Care Advocate Team now.